Medicare’s Stance on Weight Loss Drugs: A Shift in Policy?
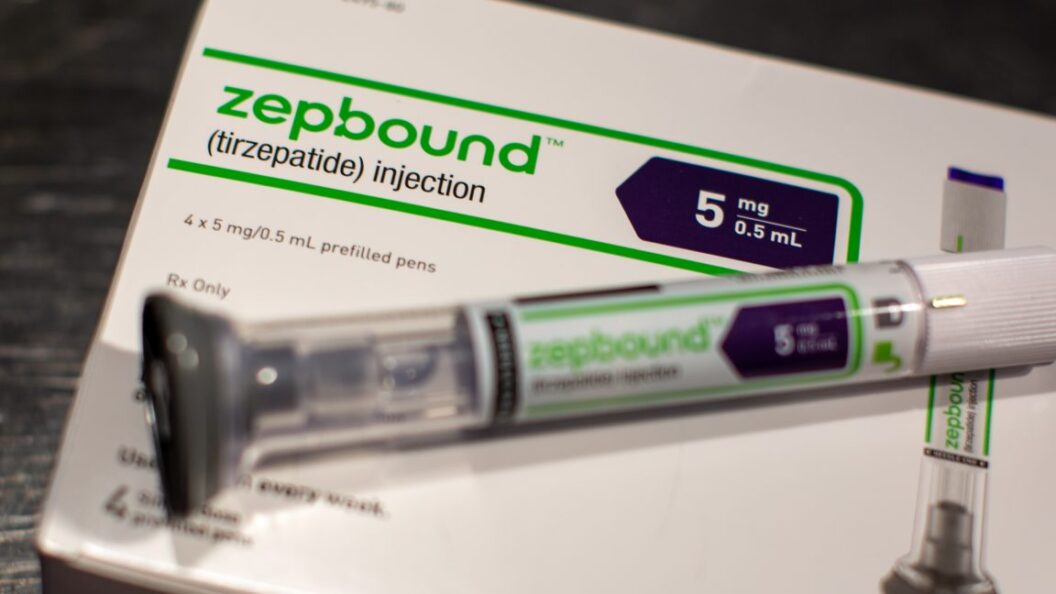
Recent discussions surrounding the coverage of prescription weight loss medications by Medicare highlight a evolving landscape in healthcare policy. Currently, Medicare does not cover medications prescribed solely for weight loss purposes. However, it does provide coverage for certain GLP-1 medications when prescribed for related health conditions, particularly Type 2 diabetes and associated cardiovascular risks.
Current Coverage Limitations
Currently, drugs like Wegovy, which falls within the GLP-1 class, can be reimbursed by Medicare if prescribed to help mitigate the risk of heart diseases in patients diagnosed with obesity or overweight. This means that patients may receive assistance in paying for these medications if their use is linked to serious health concerns, but not if their primary purpose is weight loss.
The Biden administration has contested this framework, proposing modifications to Medicare’s interpretation of prescription coverage that would encompass "anti-obesity medications." This move aims to widen access to these drugs, which could play a critical role in addressing obesity in the American population.
Industry Advocacy for Expanded Coverage
As pharmaceutical companies advocate for broader coverage, Lilly’s CEO has made it clear that the company intends to engage with the Trump administration regarding policy changes. One primary argument is the potential long-term savings on healthcare costs through the improved health outcomes provided by early intervention with medications like GLP-1 drugs.
In a statement made to Bloomberg, CEO David Ricks highlighted this position: "My argument to Mehmet Oz is that if you want to protect Medicare costs in 10 years, have [the Affordable Care Act] and Medicare plans list these drugs now. We know so much about how much cost savings there will be downstream in heart disease and other conditions." This strategy underscores the push for a preventive health approach that could inherently affect Medicare’s budget over time.
Contrasting Perspectives on Financial Impact
However, skepticism remains regarding the fiscal implications of these proposed changes. An October report from the Congressional Budget Office (CBO) strongly disputed the assertion that expanded coverage for anti-obesity medications would yield significant cost savings. The CBO projected that from 2026 to 2034, the direct costs associated with Medicare coverage for anti-obesity drugs could reach nearly $39 billion, while the expected savings from improved health outcomes would only total a little over $3 billion, resulting in a net cost of approximately $35.5 billion to taxpayers.
The Debate Over Healthcare Cost and Coverage
This divergence in perspectives illustrates a significant debate in healthcare policy—balancing immediate healthcare costs against potential long-term savings from improved health. Advocates for broader medication coverage argue that investing in preventative care could not only lead to healthier populations but also reduce costs associated with treating chronic and severe conditions connected to obesity. Opponents, including some policymakers and financial analysts, warn that the financial burden of widespread drug coverage could outweigh any anticipated benefits.
Conclusion: A Critical Intersection of Policy and Health
As the Biden administration evaluates the potential to expand Medicare’s prescription coverage to include weight loss drugs, there lies a crucial intersection of health policy and fiscal responsibility. The ongoing dialogue reflects broader societal discussions about obesity management, healthcare costs, and the role of government in regulating and supporting public health initiatives.
Whichever direction the policy takes, it will undoubtedly have significant implications for millions of Americans facing obesity and associated health risks. As this issue continues to unfold, it will be essential for stakeholders—including healthcare providers, policymakers, and patients—to engage in informed discussions about both the benefits and challenges of such a transformative shift in Medicare’s approach to prescription drug coverage.